Streamlining Complex Case Management: How Referral Networks Can Improve Chronic Disease Care
Chronic diseases, like obesity and diabetes, affect an estimated 129 million Americans, and many of those patients live with more than one condition.
And coordinating care for patients with multiple chronic health conditions is anything but simple. Between navigating specialities, managing fragmented records, and avoiding duplicate tests, complex case management can feel like a logistical nightmare.
But when referral networks are connected and intelligently designed, they can help providers cut through the chaos. This article examines how advanced referral systems are streamlining communication, enhancing outcomes, and alleviating the burden on care teams.
What Is Complex Case Management?
Complex case management involves the coordinated oversight of patients with multiple chronic conditions—those who often consult with several specialists, take numerous medications, and require ongoing care across various settings.
It’s a high-tough process that demands personalized planning, frequent communication, and detailed follow-through.
The challenge with complex case management is that patients often fall through the cracks. With information scattered across systems and providers operating in silos, care becomes fragmented. Specialists may not be aware of what others have prescribed or recommended. Tests are duplicated, appointments are missed, and care teams spend hours chasing down updates. For patients with chronic illnesses, the stakes are high, and so is the potential for error.
This is why effective complex case management is essential. Done right, it improves quality of life, reduces hospitalizations, and lowers healthcare costs. But to do it well, care teams need better tools, like patient referral networks, to stay connected.
The Role of Referral Networks in Chronic Disease Care
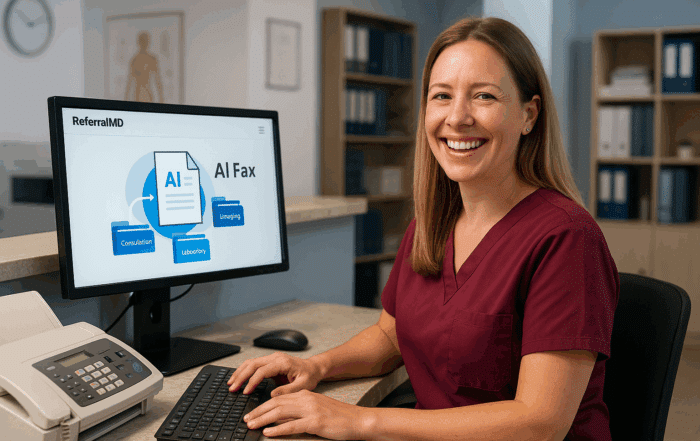
A referral network is a digital infrastructure that connects providers, specialists, and support services across the continuum of care. Unlike traditional referral processes that rely on faxes, phone calls, and guesswork, modern referral networks automate and streamline handoffs between care settings.
Enhanced Care Coordination
When providers are connected through a referral network, patients experience smoother transitions between appointments and fewer gaps in care. That sense of continuity boosts both adherence and satisfaction. Instead of repeating their story at every stop, patients know their care team is on the same page.
For example, mesothelioma cancer, known for its complexity and aggressive nature, requires comprehensive and coordinated care to improve patient outcomes. Streamlining case management through well-established referral networks is essential in managing such chronic and challenging diseases.
These networks connect patients with specialists in oncology, pulmonology, and palliative care, ensuring timely access to expert diagnostics, advanced treatments, and supportive services. By leveraging referral networks, healthcare providers can facilitate communication and collaboration, thereby reducing delays and enhancing the quality of care for mesothelioma patients who simultaneously navigate multiple medical needs.
Reduced Administrative Burden
The ultimate goal of referral networks is to streamline the patient experience and health outcomes. But they also lighten the load for care teams.
Automated workflows replace time-consuming manual processes, such as faxing referrals or making phone calls to confirm appointments. With fewer follow-ups falling through the cracks, staff can focus on more meaningful interactions.
To get the complete picture of how referral networks can reduce the strain on care teams, imagine a scenario where a physician refers a patient with congestive heart failure to cardiology, nutrition, and physical therapy.
Thanks to a referral network, each specialist automatically receives relevant records. The platform can also confirm appointment scheduling and alert staff if any steps are missed. This eliminates the back-and-forth that would typically tie up hours of administrative time per patient.
Core Features of an Effective Referral Network
To support complex case management, a referral network must offer more than basic connectivity. Here are the core features that make the difference.
Secure Information Sharing
HIPAA-compliant data exchange is foundational to trust and efficiency. An effective referral network enables providers to securely share clinical notes, diagnostic test results, imaging, and care plans in real-time. Instead of relying on fax documents or outdated email chains, care teams can access the exact information they need, when they need it. This ensures that no one is operating in the dark and reduces the risk of redundant or conflicting care directions. For patients with chronic medical conditions, it means fewer repeated tests and more informed treatment plans across the board.
Automated Tracking and Reminders
One of the most significant points of failure in traditional referral networks is the follow-up. A referral may be sent, but without tracking, it’s easy for patients to miss appointments or for providers to assume someone else is handling the next step.
A modern referral network eliminates that uncertainty. It tracks the status of every referral from initiation to completion, sending automated reminders to both patients and providers along the way.
For example, if a specialist hasn’t scheduled an appointment or a patient doesn’t follow through, the system can flag it for follow-up. This helps reduce delays, improve adherence, and help keep patients on course.
So, when looking for a referral platform, look for systems that provide:
- Customizable workflows based on referral type, provider role, or patient priority
- Escalation alerts if a referral remains unaddressed beyond a set timeframe
- Patient self-scheduling options linked directly from reminders to reduce back-and-forth
- Two-way messaging between referring and receiving providers to confirm handoff and clarify needs
Real Time Analytics and Reporting
You can’t improve what you don’t measure. That’s why robust analytics tools are critical in any effective referral network.
With real-time dashboards, healthcare organizations can monitor referral volumes, track turnaround times, measure appointment completion rates, and pinpoint where delays or drop-offs occur most frequently. As a result, care coordinators and administrators can troubleshoot bottlenecks, reallocate resources, and refine workflows over time.
When it comes to complex care management, this visibility translates to more responsive care, faster interventions, and ultimately, better outcomes for patients navigating multiple conditions. Consider integrating a coworking app to enable care coordinators to streamline collaboration and task management across various teams.
Conclusion
Complex case management is essential for patients with chronic diseases, but without the proper infrastructure, it can overwhelm even the best care teams.
Referral networks bring clarity, speed, and structure to the process, which helps providers deliver better outcomes with less effort.
Discover how ReferralMD can streamline your organization’s workflows with more innovative, simpler solutions designed for complex care. Schedule a demo today.
About the Author
Kelly Moser is the co-founder and editor at Home & Jet, a digital magazine for the modern era. She’s also the content manager at Login Lockdown, covering the latest trends in tech, business, and security. Kelly is an expert in freelance writing and content marketing for SaaS, Fintech, and e-commerce startups.